In recent years, attention to sterile processing and instrument care has grown beyond hospitals and large clinics to include outpatient centers, dental practices, veterinary clinics, and small surgical suites. As healthcare teams seek packaging solutions that are both reliable and easy to use, self-sealing sterilization pouches have become a notable option.
Content
- 1 What is a self-sealing sterilization pouch?
- 2 How the design supports sterilization processes
- 3 Practical advantages for healthcare teams
- 4 Use cases and environments where pouches fit well
- 5 Best practices for effective use
- 6 Addressing common concerns
- 7 Comparative snapshot: pouches versus rigid trays and wraps
- 8 Training and compliance considerations
- 9 Economic considerations
- 10 Real world adoption patterns
- 11 Environmental and supply chain notes
- 12 How Hopeway AMD positions its offering
- 13 Integrating a new tool into patient-care systems
What is a self-sealing sterilization pouch?
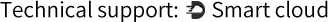
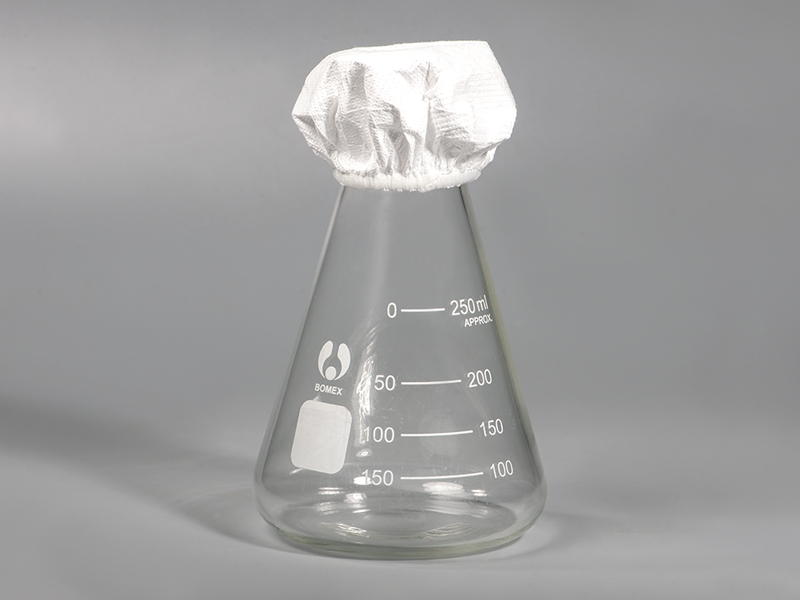
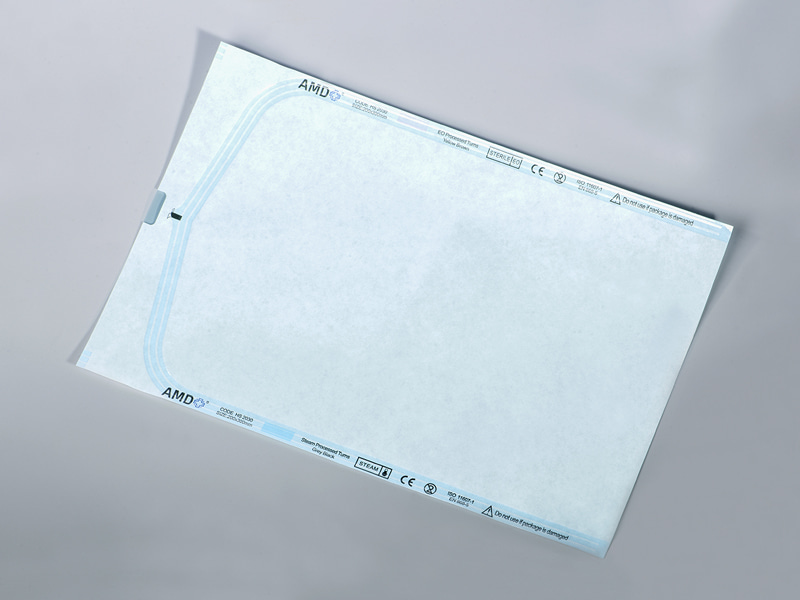
A self-sealing sterilization pouch is a single-use, barrier package designed to hold instruments during sterilization cycles and until the point of use. It combines a flexible film with a permeable backing so sterilant can penetrate the package and then keeps the contents protected once the cycle is complete. Self-adhesive closures eliminate the need for heat-sealing equipment in many settings, simplifying the packaging step while maintaining a controlled sterile environment when handled correctly.
How the design supports sterilization processes
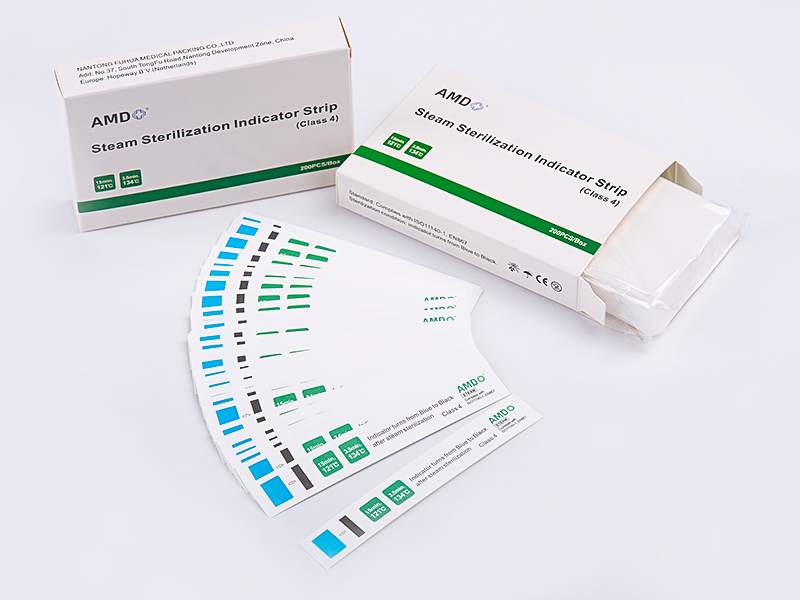
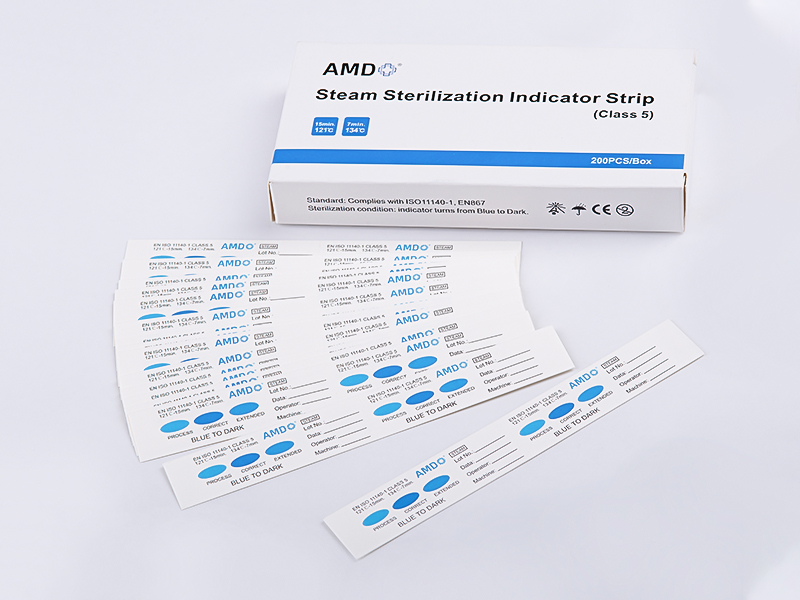
At the core of these pouches is a balance between permeability and protection. The material allows sterilizing agents — such as steam, ethylene oxide, or other compatible methods — to reach instruments during processing, while forming a secure barrier afterward. The adhesive closure is specifically engineered to remain sealed under typical storage and handling conditions yet allows easy opening by the clinician at the point of use. Features commonly highlighted in practice include:
- Clear windows or transparent film for easy instrument identification without breaking the seal.
- Permeable backing materials that allow sterilant entry and drying during steam cycles without trapping moisture.
- Tamper-evident or easily checked seals so staff can confirm package integrity quickly.
- Compatibility with routine sterilization methods when used as directed.
These design elements work together to make sterilization cycles predictable and handling straightforward, especially in facilities that prefer small batches or where a sealer machine is not available.
Practical advantages for healthcare teams
Several operational benefits contribute to the growing adoption of self-sealing pouches in a variety of care settings.
Streamlined workflow
Removing the need for an external heat sealer reduces equipment requirements. For practices that process small instrument volumes, the packaging stage becomes quicker: instruments are wrapped, pouch adhesive is engaged, and the packaged set moves directly to sterilization. This can reduce training overhead for staff and lower the barrier to maintaining a standardized packaging protocol.
Enhanced traceability and organization
Transparent film panels support visual inspection and reduce time spent searching for specific items. When combined with clear labeling practices, the pouch makes instrument tracking simpler during storage and retrieval, which benefits inventory control and audit processes.
Reduced space and capital requirements
Without dependence on tabletop sealing devices, facilities save bench space and capital expenditure. For satellite clinics or mobile units, the portability and simplicity of adhesive closures can be a decisive advantage.
Consistency across sterilization modalities
The right pouch formulation can be compatible with several sterilization methods, allowing a unified packaging approach across mixed environments. That consistency aids process validation and helps teams maintain coherent protocols.
Safer handling and point-of-use readiness
A well-designed pouch can protect instruments from contamination during storage and transit. When staff open the package at the point of care, the sterile field is more predictable, provided handling follows recommended practices.
Use cases and environments where pouches fit well
Self-sealing packaging is well suited to scenarios where instrument sets are small, turnaround time matters, or where a facility seeks to simplify sterile processing without sacrificing control. Typical environments include:
- Dental operatories managing hand instruments and small sets.
- Outpatient procedure rooms where flexible packaging is more practical than rigid trays.
- Veterinary clinics that process instruments in smaller quantities.
- Remote or field medical units that require portable, low-equipment solutions.
- Specialty clinics that package single instruments for immediate or scheduled use.
In larger central sterile departments, pouches still have value for single instruments or specialty devices that benefit from individual packaging.
Best practices for effective use
To derive the expected benefits, facilities should integrate pouches into existing sterile processing systems rather than treating them as a shortcut. Key practices include:
- Staff training: Ensure everyone packaging instruments understands loading orientation, how to engage the seal correctly, and the importance of not overfilling the pouch.
- Proper labeling: Date, contents, and sterilizer load information should be recorded on the pouch to facilitate traceability and compliance.
- Storage conditions: Packaged items should be stored in a clean, dry environment away from high traffic or contamination risks.
- Regular inspection: Pouches should be visually checked for seal integrity and package damage before use.
- Compatibility checks: Confirm that the chosen pouch is suitable for the sterilization modality used in your facility and that validation steps are documented in policy.
Adherence to these practices ensures that the packaging contributes to patient safety and regulatory compliance rather than introducing risk.
Addressing common concerns
Healthcare teams often raise predictable questions when considering a transition to self-sealing pouches. Here are concise responses to typical concerns.
- Seal reliability: Modern adhesive technologies are engineered for secure closure under normal storage conditions. Choosing a product from a reputable supplier and following manufacturer packing instructions helps maintain consistency.
- Sterilant penetration and drying: Proper pouch material selection and correct loading support sterilant access and drying. Overpacked pouches or incorrect placement in the sterilizer can impede performance and should be avoided.
- Shelf life: Many pouches are designed for extended storage; however, packages should be stored according to guidelines. Damaged or compromised packages must be discarded.
- Environmental impact: Single-use packaging raises sustainability questions. Some facilities offset by optimizing inventory, reducing waste through correct sizing, and using recycling programs where applicable.
Comparative snapshot: pouches versus rigid trays and wraps
| Criterion | Self-sealing pouch | Rigid tray | Wrapping systems |
|---|---|---|---|
| Equipment requirements | Minimal | High (tray sterilizers, racks) | Moderate (sealers, wrappers) |
| Best for | Single instruments, small sets | Complex procedure sets, large trays | Medium sets, hospital central sterile |
| Visibility of contents | High | Variable | Low unless labeled |
| Portability | High | Low | Moderate |
| Turnaround flexibility | High | Lower | Moderate |
Training and compliance considerations
Rolling out a new packaging option should be accompanied by clear documentation and competency checks. Sterile processing should be guided by institutional policies and by applicable national and international standards. Key actions include:
- Updating procedural manuals to reflect pouch use and labeling conventions.
- Including pouch packaging in staff competency assessments.
- Recording process validation steps and maintenance logs for sterilization equipment.
- Performing routine audits to verify adherence to packaging protocols.
When documentation and training align, packaging choices like self-sealing pouches become effective tools rather than variables that complicate compliance efforts.
Economic considerations
From an operational standpoint, switching packaging formats influences cost structures in multiple ways. Immediate savings may arise from avoided capital purchases and lowered maintenance costs. However, unit cost of consumables and waste disposal should be incorporated into a full cost analysis. Facilities should evaluate:
- Average instrument throughput and packaging unit costs.
- Equipment maintenance and depreciation avoided by reducing machine purchases.
- Labor time saved in packaging steps and in instrument retrieval at point of care.
- Inventory management effects, including storage footprint and stock rotation.
A short pilot program can provide local data for decision makers to model total cost of ownership and operational impact.
Real world adoption patterns
Across ambulatory and specialty sectors, teams that adopt self-sealing pouches tend to favor settings with lower daily instrument volumes or where mobility and simplicity are priorities. Larger institutions may use them selectively for specific implantable device packaging or for instruments that benefit from individual wrapping. Experience shows that clear policies and consistent staff training accelerate successful implementation and help avoid errors that might otherwise arise from misapplication.
Environmental and supply chain notes
Sustainability and supply continuity are important considerations. When evaluating vendors, procurement teams often look at material recyclability, packaging minimalism, and the vendor's ability to meet ongoing supply needs. Diversifying sources and establishing reliable par levels helps prevent interruptions that can affect patient care.
How Hopeway AMD positions its offering
Hopeway AMD's Sterilization Self Sealing Pouch is presented for healthcare buyers who value simplicity and predictable handling. The product discussion emphasizes compatibility with standard sterilization protocols and practical features that aid daily use. Importantly, institutions should always confirm compatibility with their sterilization equipment and quality assurance processes when incorporating a new package format into clinical practice.
Integrating a new tool into patient-care systems
Packaging in sterile processing is more than a commodity choice. It affects storage, instrument lifecycle, staff workflow, and ultimately how reliably caregivers can access sterile tools at the point of care. Self-sealing pouches provide an option that blends convenience with established sterilization science. When facilities pair the right material with disciplined technique, transparent labeling, and routine quality checks, the approach can reduce complexity and support consistent, efficient practices across a range of care settings.
For procurement teams and clinical leaders considering a change, the recommendation is to pilot the pouch in a limited scope, gather staff feedback, and measure impacts on time, cost, and handling. Doing so yields practical evidence for broader adoption decisions and helps ensure that packaging choices align with patient-safety goals and regulatory expectations.

 English
English Français
Français Deutsch
Deutsch Nederlands
Nederlands








 ‘s-Gravenweg 542, 3065SG RotterdamThe Netherlands
‘s-Gravenweg 542, 3065SG RotterdamThe Netherlands
 +31 (0)10 254 28 08
+31 (0)10 254 28 08