Sterilization self-sealing pouches are a common sight in clinics, dental offices, and sterile processing departments. At glance they look simple — clear film on one side, paper on the other, and a peel-and-press closure — but their design hides a careful balance of materials, sterilant access and barrier protection.
Content
- 1 What they are made of (and why that matters)
- 2 The sealing mechanism: effortless closure, reliable result
- 3 How sterilization actually occurs inside the pouch
- 4 Built-in indicators and visual checks
- 5 Practical workflow: from loading to unpacking
- 6 Pros and considerations
- 7 Common mistakes to avoid
- 8 Environmental factors: moisture, humidity and temperature
- 9 Physical stresses: puncture, abrasion and improper handling
- 10 Sterilization process mismatch and monitoring
- 11 Storage threats: dust, pests and transport vibration
- 12 Human and workflow factors
- 13 Chemical and environmental exposures
- 14 Time and shelf-life considerations
What they are made of (and why that matters)
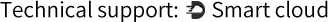
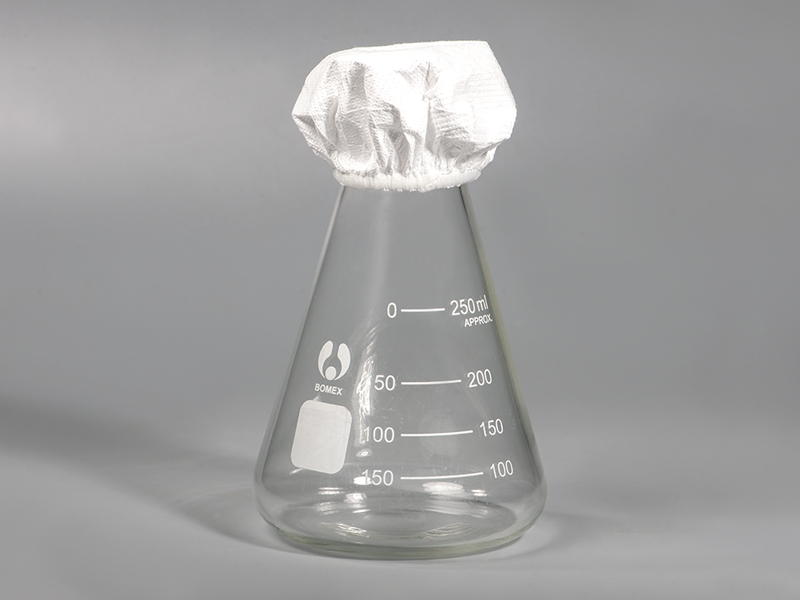
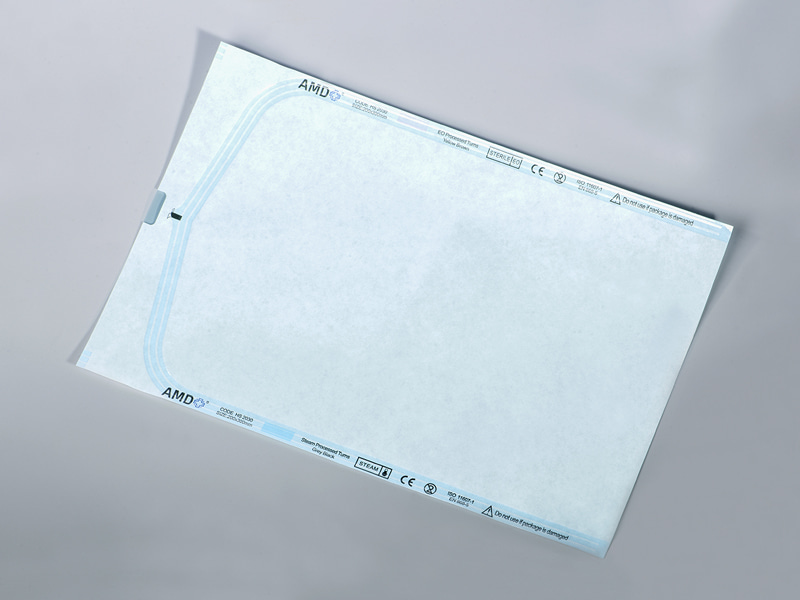
A typical self-sealing sterilization pouch combines a medical-grade paper layer with a transparent polymer film. The paper is porous enough to allow sterilizing agents (steam, ethylene oxide or some low-temperature plasma gases, depending on the pouch type) to enter and exit during a cycle, while the film gives clear visibility of the contents and helps resist puncture or tearing during handling. Manufacturers select paper weights and film constructions so that the package will tolerate the sterilization environment while still forming a consistent barrier afterward. Hopeway AMD's product line, for example, pairs reinforced film with specialist medical paper to achieve that balance.
The sealing mechanism: effortless closure, reliable result
Self-sealing pouches include an adhesive strip under a removable liner or flap. To prepare a pouch, a sterile instrument — already cleaned and dried — is placed inside, the liner is peeled back, and the flap is folded and pressed to close the adhesive. No heat sealer is needed, which speeds preparation and reduces equipment dependency. Because the adhesive system is designed for predictable tack and strength, it can provide a secure closure that retains integrity during sterilization and storage when used according to the manufacturer's instructions.
How sterilization actually occurs inside the pouch
The sterilant reaches the instrument through the porous paper side. In a steam autoclave cycle, for example, steam penetrates the paper, contacts the item and achieves microbial kill according to the cycle's validated parameters. The polymer film side remains non-porous, so after the sterilant has done its work and the pouch is dried, the combination of paper and film forms an effective sterile barrier until the package is opened for use. Because different sterilization methods interact differently with materials, pouches are produced to be compatible with specific processes; always check the pouch label for indicated methods.
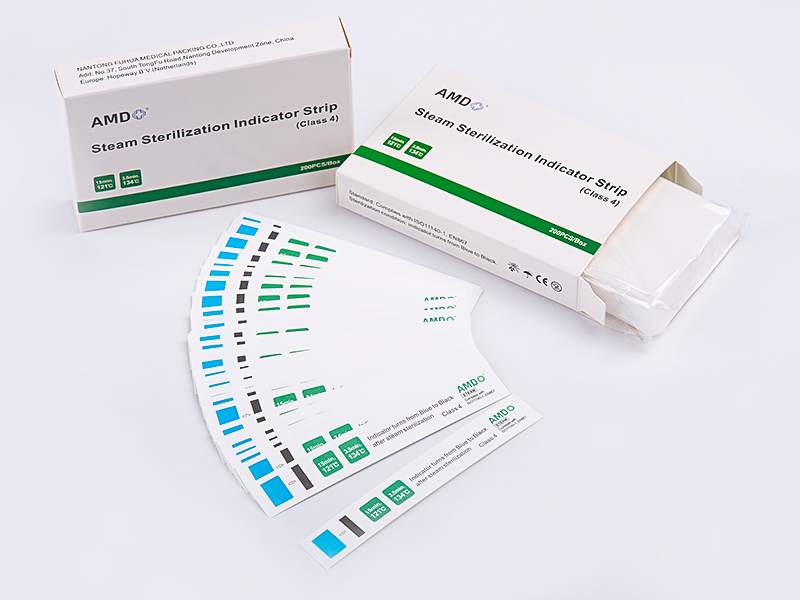
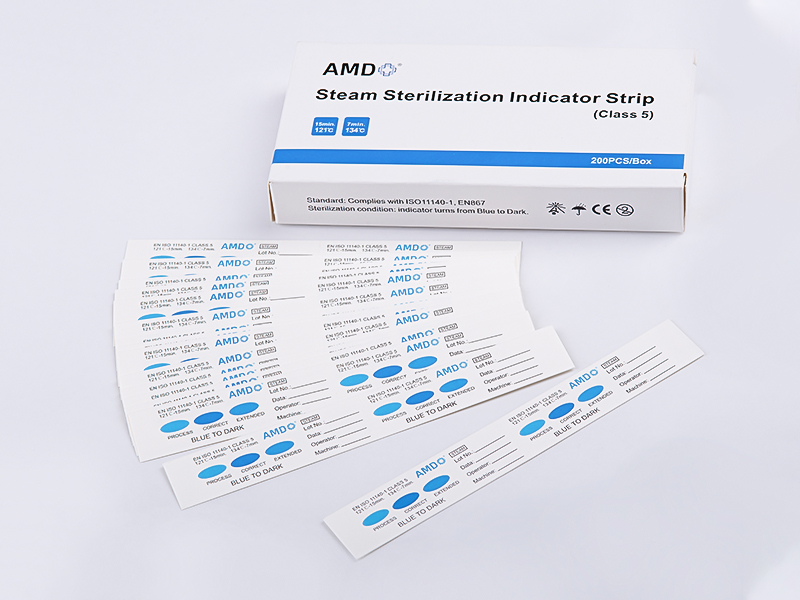
Built-in indicators and visual checks
Most modern pouches include an external chemical indicator that changes color when exposed to the appropriate sterilization conditions. These markings offer a quick visual cue that the package has been through a cycle, although they are not a substitute for biological indicators or routine monitoring required by facility protocols. Visual inspection of the package after sterilization — confirming the indicator change, checking for intact seals, and verifying the instrument inside — remains an important step before storage and later use.
Practical workflow: from loading to unpacking
Clean and dry instruments thoroughly (moisture or residues can interfere with sterilization).
Place the instrument inside the pouch without overstuffing; items should lie flat.
Remove the liner and press the adhesive flap firmly to seal.
Arrange pouches in the sterilizer according to the device manufacturer's loading instructions.
After the cycle and adequate drying, inspect indicators and seals before storing.
When opening, peel the film from the paper to present instruments aseptically; the peel-open action helps prevent contamination of the device prior to use.
Pros and considerations
| Feature | Self-sealing pouches | Heat-sealed pouches |
|---|---|---|
| Speed of preparation | Fast — no sealer needed | Requires heat sealer and warm-up |
| Equipment dependence | Minimal | Requires specialized equipment |
| Seal uniformity | Good when used correctly | Often very uniform and flat |
| Fit | Small instruments, rapid throughput | Heavy duty needs, batch sealing |
Common mistakes to avoid
Using a pouch for instruments that are wet or contaminated with residue.
Over-filling the pouch so that the adhesive cannot form a continuous seal.
Subjecting pouches to sterilization methods they are not designed for.
Relying solely on chemical indicators without regular biological monitoring and documented process controls.
Environmental factors: moisture, humidity and temperature
Excess humidity or direct moisture can soften paper, reduce adhesive tack, and encourage microbial growth if storage conditions are poor. High temperatures or repeated temperature cycling can age adhesives or change film flexibility, increasing the chance of cracks or seal failure. For these reasons, sterilized packs should be stored in a clean, dry area at stable room conditions and handled so seals are not stressed. National guidance and sterilization practices emphasize appropriate storage and labeling to preserve package integrity.
Physical stresses: puncture, abrasion and improper handling
Sharp instruments, rough edges of trays, or abrasive movement during transport can puncture the film or tear the paper layer. Overstuffing a pack or folding plastic layers over each other also increases the risk of mechanical damage and can prevent adequate sterilant penetration. Careful instrument preparation — choosing the correct pack size, using protective trays or instrument guards, and avoiding overfilling — reduces these mechanical risks. Industry resources and clinical practice notes routinely call out handling errors as preventable causes of failure.
Sterilization process mismatch and monitoring
Using a pack with a sterilization method for which it was not validated (for example, a pouch designed for steam placed in a low-temperature plasma cycle) can go to inadequate sterilant penetration or material degradation. Internal chemical indicators help show that sterilant reached the contents; external process indicators and periodic biological monitoring complete the assurance picture. Facilities should follow the sterilizer and packaging manufacturers' compatibility guidance and maintain a monitoring program aligned with regulatory recommendations.
Storage threats: dust, pests and transport vibration
Packages left in dusty, damp or pest-prone areas can be physically contaminated or weakened. Vibration during transport — especially if packs are loosely packed in boxes — can abrade seals over time. Central sterilization standards recommend dedicated storage areas, proper shelving, and inventory practices (rotation, labeling and quarantining suspect loads) to reduce these risks.
Human and workflow factors
Human error is a frequent contributor: failing to dry instruments before packing, skipping the chemical indicator, peeling liners incorrectly, or using a pouch more than once. Training, clear standard operating procedures and ergonomic workflows (so staff are not rushing or working in cramped areas) help reduce mistakes that compromise package integrity. Root cause analyses of packaging failures repeatedly point to process and training gaps as actionable fixes.
Chemical and environmental exposures
Contact with solvents, corrosive cleaning residues, or strong disinfectants can degrade paper, film or adhesive. Additionally, prolonged exposure to sunlight or UV sources can embrittle some films. Keep processed packs away from cleaning agents, chemical storerooms, or direct sunlight; follow manufacturer guidance on permissible exposures.
Time and shelf-life considerations
While many sterile packs remain effective under "event-related" sterility principles, aging of adhesives or accidental handling over long storage periods may eventually compromise a seal. Facilities should adopt storage timelines in line with manufacturer instructions and local policy, inspect packs before use, and label packages with sterilization dates and batch identifiers to support traceability.
Self-sealing sterilization pouches combine simple handling with engineered materials to create an effective sterile barrier system. By pairing the right pouch with validated sterilization cycles, following manufacturer instructions, and performing routine monitoring, healthcare teams can use these packs to support safe instrument management and efficient workflows. If you use a particular brand or model, review its instructions for use and compatibility details to ensure it matches your sterilization equipment and clinical needs.

 English
English Français
Français Deutsch
Deutsch Nederlands
Nederlands








 ‘s-Gravenweg 542, 3065SG RotterdamThe Netherlands
‘s-Gravenweg 542, 3065SG RotterdamThe Netherlands
 +31 (0)10 254 28 08
+31 (0)10 254 28 08