In medical and dental environments, instruments are repeatedly used and therefore require a controlled reprocessing cycle before returning to service. After cleaning and disinfection, a protective barrier is necessary to keep items isolated from external contamination until the moment of use. This barrier is not merely a wrapper; it functions as a safeguard that supports infection prevention workflows and helps maintain confidence during procedures.
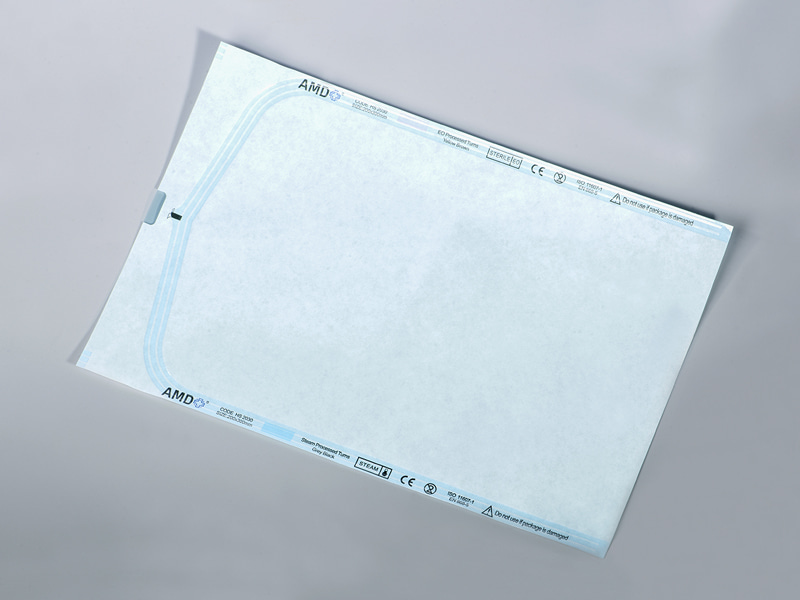
A Heat Sealing Sterilization Pouch is one such packaging solution designed to hold medical tools after preparation and before application. It forms a sealed enclosure that allows sterilizing agents to enter and exit while helping preserve internal cleanliness during storage and transport.
Content
- 1 Why Packaging Matters After Sterilization
- 2 Core Structure and Materials
- 3 How Heat Sealing Works
- 4 Supporting Aseptic Presentation
- 5 Applications Across Healthcare Settings
- 6 Storage and Handling Considerations
- 7 Environmental Awareness
- 8 Step One: Preparing the Instruments
- 9 Step Two: Selecting the Appropriate Pouch
- 10 Step Three: Performing the Heat Seal
- 11 Step Five: Storage and Handling
- 12 Step Six: Aseptic Opening
- 13 Training and Workflow Consistency
- 14 Maintaining Cleanliness After Processing
- 15 Supporting Organized Workflows
- 16 Safe Storage and Transportation
Why Packaging Matters After Sterilization
Sterilization alone does not guarantee safety if an instrument becomes exposed afterward. Once processed, tools can easily contact air particles, handling surfaces, or storage containers. Without protection, the effectiveness of the sterilization cycle may be compromised.
Packaging provides a controlled boundary. The sealed structure works as a microbial barrier, supporting hygienic storage until the moment a clinician opens it. In practice, this helps create a predictable workflow: prepare, sterilize, store, and present instruments in a consistent manner. Healthcare facilities rely on such routines because predictability reduces uncertainty and supports patient care.
Core Structure and Materials
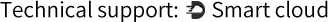
Sterile pouches are typically constructed using a combination of medical-grade paper and transparent film. The paper side permits sterilizing media to pass through during processing, while the transparent side allows staff to view the enclosed items without opening the package.
This design has practical value. Staff can confirm instrument presence and arrangement at a glance. The sealed edges form a secure enclosure once heat is applied, creating a defined peel opening that supports aseptic presentation. When opened correctly, the contents can be transferred to a sterile field without unnecessary contact.
The material selection is intentional. It balances permeability with containment, allowing sterilizing vapor to circulate while helping prevent external particles from entering after processing.
How Heat Sealing Works
Heat sealing uses controlled pressure and temperature from a sealing device to bond the edges of the pouch. The process softens a thin layer within the packaging material, creating a uniform seal line. Once cooled, the bond remains stable under normal handling conditions.
A consistent seal is important. If the seal is incomplete, the barrier may not function as intended. If the seal is excessive, opening the pouch may become difficult and could risk contaminating the instrument during removal. Proper technique and equipment maintenance therefore play a meaningful role in routine clinical operations.
Supporting Aseptic Presentation
One of the often overlooked aspects of sterile packaging is presentation. The moment the package is opened is a critical point in the workflow. The peelable design helps the user separate the film from the paper without shaking or touching the instrument directly.
The clear side also assists in positioning. Clinicians can orient tools before opening, reducing unnecessary movement and supporting organized preparation. These small procedural details contribute to an orderly environment in treatment areas.
Applications Across Healthcare Settings
Sterile pouches are used in a wide range of settings. Dental clinics package hand instruments before appointments. Surgical departments prepare smaller devices for procedures. Outpatient centers maintain prepared trays for daily operations. Even educational training facilities adopt these practices to teach correct handling techniques.
Although the environments differ, the purpose remains the same: maintain cleanliness from processing to point of use. Consistency across departments helps staff adapt quickly when working in different treatment rooms or assisting various professionals.
Storage and Handling Considerations
After sealing and sterilization, storage conditions also matter. Packages are typically placed in clean, dry areas away from excessive handling. Organized shelving or cabinets allow staff to retrieve instruments without bending, crushing, or stacking them improperly.
Handling discipline is important. Even a well-sealed pouch can be compromised if punctured by sharp tools or pressed against rough surfaces. Many facilities implement simple visual inspection routines. Staff check for seal integrity, discoloration, or visible damage before presenting an instrument.
Environmental Awareness
Modern healthcare increasingly pays attention to environmental impact. Packaging materials are therefore designed with practical balance in mind: durability for safe handling while avoiding unnecessary bulk. Proper waste segregation and disposal procedures help facilities align with local regulations and sustainability practices.
Training staff in correct usage also reduces waste. When the correct pouch size is chosen and sealed properly, the likelihood of reprocessing decreases. Thoughtful selection and routine instruction support efficient resource use.
Instrument reprocessing in healthcare settings follows a structured path: cleaning, inspection, packaging, sterilization, storage, and clinical use. Each stage depends on the previous one. If any step is overlooked, the entire process may lose reliability. Among these stages, packaging is sometimes underestimated, yet it plays a practical role in maintaining hygiene after instruments leave the sterilizer.
A Heat Sealing Sterilization Pouch is designed to hold prepared instruments in a sealed environment after processing and before use. Understanding how it functions in real working conditions helps staff perform consistent procedures and supports organized clinical routines.
Step One: Preparing the Instruments
Before packaging begins, instruments must be thoroughly cleaned. Residues, debris, and moisture should be removed so the sterilization cycle can act effectively. Staff typically rinse, brush, and dry items according to facility protocols. Once clean, tools are inspected for damage, alignment, and surface condition.
Inspection is an important stage. Packaging an instrument that is bent, cracked, or still damp may cause complications later. Moisture trapped inside the pouch can affect the sterilization process, while damaged instruments may puncture the packaging. Careful preparation therefore protects both the device and the packaging material.
After inspection, the instruments are arranged in an open position when possible. Hinged tools are not locked shut so sterilizing media can reach all surfaces.
Step Two: Selecting the Appropriate Pouch
Choosing the correct size is part of effective packaging. A pouch that is too small may stress the seal area, while one that is too large allows unnecessary movement during handling. Instruments should lie flat without bending or forcing the edges.
The transparent side allows visual confirmation of the contents, while the medical paper side allows sterilizing agents to circulate during processing. Staff place instruments carefully so sharp tips do not touch the seal area. In some facilities, protective tip covers are used to reduce the chance of punctures.
Clear identification also helps organization. Many departments write the processing date or instrument name on the designated labeling area, avoiding the seal line.
Step Three: Performing the Heat Seal
The sealing stage requires a controlled device that applies temperature and pressure. The open edge of the pouch is inserted into the sealer, and a straight seal line is created. The goal is a continuous bond across the entire width of the pouch.
The seal must remain even. If wrinkles or gaps appear, the barrier may not function as intended. Staff often perform a quick visual inspection immediately after sealing to confirm the line is uniform and intact.
Routine equipment checks are also part of the process. Clean sealing bars and stable temperature settings help produce consistent seals. Training and practice allow staff to recognize acceptable results.
Step Four: Sterilization Cycle
After sealing, the packaged instruments are placed inside the sterilizer. The pouch is positioned so the paper side faces the sterilizing medium when required by facility guidelines. Space is left between packages to allow circulation.
During the cycle, sterilizing vapor or gas penetrates through the medical paper layer and reaches the instruments. After processing, the contents are free from viable microorganisms under proper conditions. The pouch then becomes a protective barrier that helps maintain cleanliness during storage.
Once the cycle finishes, packages are allowed to dry and cool before handling. Moving them while warm may affect the seal or allow moisture to form.
Step Five: Storage and Handling
After sterilization, the packaged instruments are transferred to a clean storage area. Shelves or cabinets are used to avoid bending and pressure. Staff handle the packages carefully, touching mainly the outer surfaces rather than the seal line.
Before use, each pouch is visually checked. Staff look for tears, punctures, or incomplete seals. If damage is observed, the instrument is reprocessed rather than used.
Proper storage also involves minimizing repeated handling. Organized labeling and clear arrangement help staff retrieve instruments efficiently without disturbing other packages.
Step Six: Aseptic Opening
When the instrument is needed, the pouch is opened in a controlled manner. The film and paper layers are peeled apart, allowing the instrument to drop onto a sterile field without direct contact. The design supports aseptic presentation and helps maintain hygiene during transfer.
Opening technique matters. Pulling slowly and steadily reduces sudden movement and helps prevent accidental contamination. The transparent film allows the clinician to orient the instrument before opening, which supports smoother preparation.
Training and Workflow Consistency
Using sterile packaging effectively depends on staff training and routine practice. Facilities often establish written procedures describing cleaning, sealing, labeling, and storage. When every team member follows the same method, the workflow becomes predictable and easier to monitor.
Regular instruction ensures new staff members understand why each step matters. Rather than viewing packaging as a simple wrapping task, they recognize it as part of infection prevention measures.
A Heat Sealing Sterilization Pouch is used as a protective enclosure for instruments after they have been processed. Its purpose is to maintain the condition of prepared tools from the moment sterilization ends until the moment they are needed in a procedure.
Maintaining Cleanliness After Processing
Sterilization removes microorganisms during the processing cycle, but exposure afterward can reintroduce contamination. A pouch forms a closed environment that helps isolate instruments from external contact. This function supports infection prevention practices and encourages consistency in handling.
By sealing the instrument inside a protective barrier, healthcare staff can transport and store items with reduced handling risk. The packaging does not replace sterilization; instead, it preserves the results of that process until clinical use.
| Aspect | Practical Use in Clinical Settings |
| Main Purpose | Maintains the prepared condition of sterilized instruments until use |
| Protection | Creates a sealed barrier against external contact during storage and transport |
| Workflow Support | Allows instruments to be prepared in advance and organized by procedure |
| Application Areas | Dental clinics, outpatient rooms, surgical preparation areas, training facilities |
Supporting Organized Workflows
Clinical environments depend on order and predictability. Staff members prepare instruments ahead of time so procedures can begin without delay. The pouch allows instruments to be processed in advance and kept ready for scheduled treatments.
The transparent film side allows the user to view the contents without opening the package. This feature supports quick identification and avoids unnecessary opening. The paper side permits sterilizing agents to enter during processing while later functioning as a microbial barrier.
By enabling preparation before appointments, packaging helps teams manage their daily schedules more efficiently and maintain a consistent workflow.
Safe Storage and Transportation
Instruments are often moved between reprocessing areas and treatment rooms. During this movement, direct exposure could occur if tools were not packaged. The sealed structure helps prevent contact with surrounding surfaces, drawers, or trays.
Storage cabinets also benefit from packaged instruments. Items can be organized and labeled while remaining enclosed. Staff can check the package condition visually before use. If the pouch shows damage or incomplete sealing, the instrument can be reprocessed.
The packaging therefore supports both transport and storage while helping maintain proper handling routines.
Sealed sterile packaging serves a practical and ongoing role in healthcare preparation. It protects processed instruments, supports organized storage, and allows controlled presentation during procedures. Rather than being a simple container, it connects reprocessing with clinical care.
By enclosing instruments after sterilization and maintaining their prepared condition until use, the pouch contributes to reliable workflows and careful handling. Through consistent application and proper technique, healthcare teams can prepare tools in advance, manage daily schedules more smoothly, and maintain orderly clinical environments.

 English
English Français
Français Deutsch
Deutsch Nederlands
Nederlands








 ‘s-Gravenweg 542, 3065SG RotterdamThe Netherlands
‘s-Gravenweg 542, 3065SG RotterdamThe Netherlands
 +31 (0)10 254 28 08
+31 (0)10 254 28 08